Introduction Immunotherapy (IO) based on anti-CD20 monoclonal antibodies significantly improves the prognosis of patients with follicular lymphoma (FL) in terms of disease progression, progression-free survival (PFS) and serious adverse events. Vaccination is protective in the general population, however, FL patients infected with COVID-19 have exacerbated damage to their immune system, and the effects of IO and vaccination on COVID-19 outcomes remain unknown. The aim of this study was to estimate the association between IO therapy based on anti-CD20 monoclonal antibody and COVID-19 severity by analyzing population-based data of FL patients. And to determine the true utility of vaccination in this immunocompromised population.
Patients and methods We retrospectively assessed the clinical characteristics and follow-up data of patients with newly diagnosed FL from December 1, 2012 to April 1, 2023 at Shandong Provincial Hospital. Patients were divided into 2 groups: those who received IO, defined as anti-CD20 immunotherapy, within 12 months prior to COVID-19 diagnosis (IO group); those who received non-IO antitumor regimens with no systemic therapy (non-IO group), defined as cytotoxic chemotherapy, targeted therapies, endocrine therapies or those who did not receive any systemic therapy. Inclusion of data on anti-CD20 immunotherapy drugs Rituximab and Obinutuzumab applied in our center, stage of treatment, etc. COVID-19 outcomes were graded primarily on the basis of hospitalization, oxygenation, and need for mechanical ventilation, and patients' overall survival (OS) as well as PFS were studied. Multivariate logistic regression analyses were performed to assess associations between variables and COVID-19 outcomes, and unadjusted odds ratios (OR) and 95% confidence intervals (95%CI) were reported.
Results Out of 160 patients included in the study ,77 (48.0%) were female, the median age was 53 (28-85 years) years, and the median follow-up was 54 (12-168 months) months. 131 (81.9%) patients had Ann Arbor stage III-IV on initial admission at our center, and 84 (52.5%) patients received the COVID-19 vaccine. Regarding COVID-19 infection, 137 (85.6%) were positive for COVID-19.
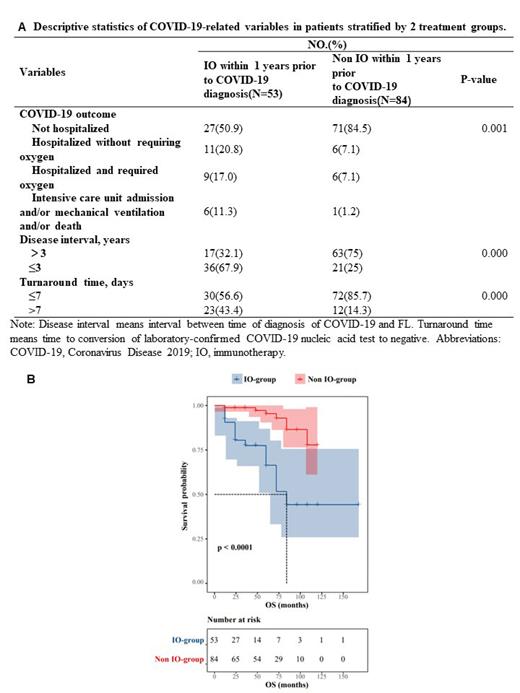
60 patients (37.5%) received IO, whereas 100 patients (62.5%) did not. Significant differences (P < 0.05) were found between the IO and non-IO groups in terms of COVID-19 outcome, time between COVID-19 diagnosis and FL diagnosis, and time to conversion after COVID-19 positivity (Figure 1A). There were also significant differences between the two groups in survival time and recurrent lung infection after COVID-19 cure (Figure 1B). No significant effect of vaccination on outcome of COVID-19 was found regardless of IO treatment.
In the IO group, 42 (70.0%) patients received Rituximab and 18 (30%) patients received Obinutuzumab. No significant differences in COVID-19 infection rate, COVID-19 clinical outcome, time to COVID-19 conversion, and survival time were found between the two drugs. Of the patients who received IO therapy, 19 (31.7%) were in the induction phase and 41 (68.3%) were in the maintenance phase. Patients receiving maintenance therapy had a greater likelihood of longer survival(P<0.0001)and less severe COVID-19 outcomes(P=0.003). Of the 60 patients treated with IO, 36 (60.0%) had an unchanged chemotherapy course and 24 (40.0%) had a delayed or interrupted chemotherapy course. No significant associations were found between IO therapeutic agents, vaccinations, or other variables with chemotherapy progression.
Conclusions Among FL patients included in the analysis, IO was associated with worse COVID-19 outcomes, but no significant correlation was found between vaccination and COVID-19 infection rates and severity at this time. These findings provide insights into the immunocompromised population of FL-combined COVID-19 patients that can be used in the clinical setting to estimate COVID-19 outcomes based on factors such as chemotherapy stage and vaccination.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal